Abstract
Background
Patients with acute myeloid leukemia (AML) have remarkable heterogeneity in the pathogenesis, clinical features, and treatment outcomes. Risk-stratification is one of the most critical factors in the treatment of these patients. Cohesin is a multimeric protein complex, composed of four core subunits, including SMC1A, SMC3, RAD21 and either STAG1 or STAG2 proteins. Studies regarding the clinical and prognostic relevance and dynamic changes of cohesin gene mutations in de novo AML patients are limited and the findings are controversial. In this study, we aimed to investigate the clinical, biological and prognostic implications of cohesin gene mutations in a large cohort of de novo AML patients.
Method
We analyzed cohesin gene mutations and their clinico-biological associations in 391 adult patients with newly diagnosed de novo non-M3 AML. To evaluate the dynamic changes of cohesin and co-occurring gene mutations, sequential analyses of gene mutations by targeted next generation sequencing using HiSeq platform (Illumina) were performed in 386 samples from 116 patients during follow-ups. Furthermore, to investigate the pathophysiological pathways associated with cohesin gene mutations, gene expression microarray analysis was performed in 173 patients, including 10 cohesin-mutated and 163 wild-type patients, who had enough mRNA for analysis.
Results
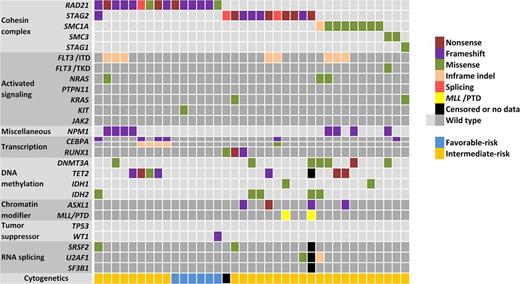
We found 37 patients (9.5%) had cohesin gene mutations, most prevalent in RAD21 (3.8%) and STAG2 (3.1%). Except for one patient with concurrent mutations in STAG2 and RAD21, the mutations in these component genes were mutually exclusive, suggesting a convergence of biological effects of these mutations (Figure 1). Mutations in STAG2 and RAD21 were mainly truncations or frameshift mutations (10/12, 83.3% and 12/15, 80%, respectively) while those in SMC1A and SMC3 were mostly missense mutations (7/8, 87.5% and 2/2, 100%, respectively). Cohesin mutations were inversely associated with complex karyotype (P=0.023) and unfavorable-risk cytogenetics (P=0.003). Interestingly, six (16.7%) of the 38 patients with t(8;21) had cohesin gene mutations, all in RAD21, while none of the patients with inv(16) had any cohesin mutation. Compared with other cohesin genes mutations, STAG2 mutations more frequently co-occurred with RUNX1 mutations (27.3% vs. 0%, P=0.023) and tended to co-occurred with ASXL1 mutations (25.0% vs. 4.0%, P=0.084), but less frequently with NPM1 mutations (0% vs. 32.0%, P=0.036) (Figure 1) . In multivariate Cox proportional hazards regression analyses for overall survival (OS) and disease-free survival (DFS), the presence of cohesin gene mutations was an independent favorable factor (P=0.047 and 0.028, respectively). A scoring system incorporating cohesin mutations and other prognostic factors could well stratify the patients into different risk groups, which could be validated in another independent cohort. Serial analyses by next generation sequencing showed that two patients lost the original cohesin mutations during disease evolution, while none of the patients without the mutation acquired a novel one at relapse. We applied Bradley-Terry model to evaluate the temporal order of gene mutations in cohesin-mutated patients. The STAG2 mutations occurred as an early event, while RAD21 and SMC1A mutations occurred relatively late. Ingenuity Pathway Analysis revealed ERK1/2 as a hub gene in cohesin mutation-associated biological pathways. Furthermore, Gene Set Enrichment Analysis demonstrated that cohesin gene mutations were closely associated with several biological pathways involved in hematopoietic/myeloid/blood cell-related functions, including differentiation of blood cells (P=7.96×10-11), proliferation of blood cells (P=3.22×10-10), apoptosis (P=1.39×10-8), and cell death of blood cells (P=9.12×10-8).
Conclusion
Cohesin gene mutations were independent prognostic factors in de novo AML. Further, cohesin gene mutations were strongly associated with the biological function related to proliferation and differentiation of blood cells. Sequential analyses showed cohesin gene mutations might be lost during disease evolution, but none of the patients without the mutation acquired a novel one during the clinical course indicating they may not be critical in disease progression. Further prospective studies with larger cohorts are warranted to confirm our findings.
Tsai: Celgene International Sàrl: Research Funding. Hou: Celgene International Sàrl: Research Funding. Tang: Celgene International Sàrl: Research Funding. Kuo: Celgene International Sàrl: Research Funding. Lin: Celgene International Sàrl: Research Funding. Yao: Celgene International Sàrl: Research Funding. Li: Celgene International Sàrl: Research Funding. Huang: Celgene International Sàrl: Research Funding. Ko: Celgene International Sàrl: Research Funding. Lin: Celgene International Sàrl: Research Funding. Wu: Celgene International Sàrl: Research Funding. Chen: Celgene International Sàrl: Research Funding. Tsai: Celgene International Sàrl: Research Funding. Tien: Celgene International Sàrl: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal